Fetal Bradycardia

Fetal bradycardia is a lowered heart rate in which the heart rate is less than 110 beats per minute (bpm) for at least 10 minutes.
The baseline fetal heart rate, or the normal fetal heart rate, is 110-160 bpm.
Bradycardia is below this baseline.
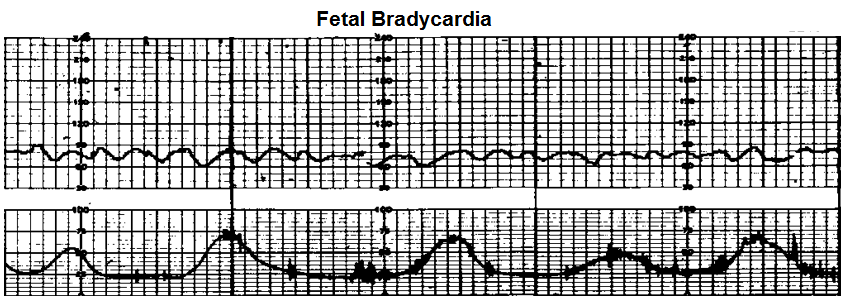
You can see from this waveform that the heart rate starts off at about 80 bpm and then elevates to 90 for a brief period of time before returning to a baseline of about 75bpm. In this strip, the heart rate goes as low as 60 bpm.
Each box represents 10 seconds of time. So each 6 boxes represents 60 seconds, or 1 minute. You can visualize 6 boxes easily by looking for the bold vertical line after each 6 boxes. All these represent 1 minute, so it's easier to visualize the complete time interval. If you count all the boxes, you will see that this graph represents 11 minutes. This is above the 10 minutes needed to diagnose fetal bradycardia.
You can see the heart rate is well below the 110 bpm for longer than 10 minutes. Thus, it's a definitive diagnosis of fetal bradycardia.
You can see that the bradycardia is constant regardless of whether is uterus is contracting or resting.
The bradycardia persists during contraction and resting periods. So it's
not correlated to the contraction cycles.
Causes of Fetal Bradycardia
Fetal bradycardia can exist for a number of reasons. Possible causes include fetal head compression, fetal hypoxia, fetal acidosis, fetal heart block, umbilical cord compression, and late second-stage labor with maternal pushing.
Fetal head compression can cause bradycardia due to vagal nerve stimulation. The vagus nerve is the 10th cranial nerve, CN X, and it interfaces with the autonomic nervous system, specifically the parasympathetic nervous system, to control the heart and digestive tract. Specially with the heart, parasympathetic innervation of the heart mediates the lowering of the heart rate. This is why stimulation of the vagus nerve, such as due to head compression, can cause bradyarrhythmias. This is why sometimes in medical practice, for patients (we're now speaking of children and adults) who have tachyarrhythmias such as atrial fibrillation, they may be trained to perform vagal manuevers. This slows down the rapid heart rate and normalizes the arrhythmia somewhat.
Fetal hypoxia and fetal acidosis can cause bradycardia or tachycardia. Bradycardia is more likely a worse sign. Because if a fetus is hypoxic and the body isn't compensating by increasing the heart rate, this is a more dire situation than if the fetus was tachycardic. In the same way, fetal acidosis with bradycardia is a worse sign as well, because the body isn't compensating for this acidotic state.
Umbilical cord compression can cause bradycardia due to vagal nerve stimulation, the same reason as for fetal head compression. While partial cord occlusion causes moderate bradycardia, complete cord occlusion causes severe bradycardia. So the more severe the cord occlusion, the greater the bradycardia. It's directly correlated to the amount of compression that there is.
Late second-state labor with maternal pushing can cause bradycardia due to hypoxia. If the mother is strenuously
pushing with adequate respirations to oxygenate her body and the fetus, this could cause fetal hypoxia. Again, the hypoxia can
cause either bradycardia or tachycardia, with bradycardia being a more serious manifestation because the fetus isn't compensating for the low oxygenated state.
Related Resources
Fetal Tachycardia- Explained
Early Decelerations- Explained
Late Decelerations- Explained
Variable Decelerations- Explained
Fetal Heart Rate Variability- Explained